


Table of Contents
ToggleIndia’s federal and state regulators recently conducted a major joint drive against manufacturers of substandard drugs in which licences of 18 companies were cancelled. The inspection was carried out across 20 states and Union Territories in India, official sources said, adding that action was taken against 76 companies in the first phase.

The move by the authorities took place in the wake of adverse reports that came from countries such as The Gambia, Uzbekistan and the US where Indian-manufactured drugs, including cough syrups and eye-drops, came under the scanner in relation to alleged deaths of children as well as adults.

Could India’s reputation as the world’s pharmacy be under threat because of these incidents abroad, particularly when the South Asian nation is making all-round efforts under the leadership of prime minister Narendra Modi to establish itself as a leading name in the international fraternity?
India Weekly spoke to Dr Sanjt Singh Lamba, managing partner of Trillyum Consulting and Advisory and chief executive officer of Biocuris Pharmaceuticals Private Limited, about the key developments related to India’s pharmaceutical sector and how he sees its functioning and what the future has in store.
Speaking about the government taking stern action against 18 pharma companies and whether India’s ‘world pharmacy’ image has come under threat by the makers of spurious drugs, Dr Lamba said the action came after three international alerts in the last three months about the quality of India-made medicines.

“Their licences have been cancelled allegedly for manufacturing spurious/substandard drugs and violating good manufacturing practices (GMPs). These incidents are regularly happening in both India market as well as exports,” he said, adding while the incident does not pose a major challenge to India’s image but the credibility has started eroding. If tough actions are not taken by the government, a bigger impact is possible in the long run, Dr Lamba said.
Even if authorities have taken action against the pharma companies that make spurious drugs after the adverse reports came from overseas, many feel it might have happened a bit late.
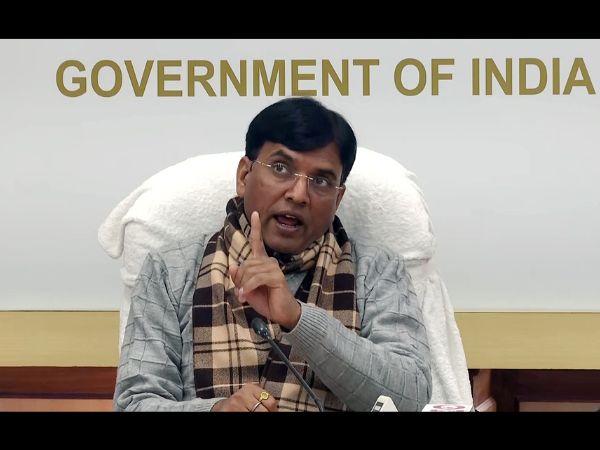
Dr Lamba also feels the same. When India Weekly asked him whether the government action was more a knee-jerk reaction or it was rightly due, he said, “This action was taken late. Mostly in the past, a political will was lacking for handling this in a tougher way. It’s expected that with new initiatives from the government and the pressure from various countries, the World Health Organisation and other regulatory agencies, action would be initiated. With the new Drugs Controller General of India, Rajeev Raghuvanshi and India’s health minister Mansukh Mandaviya stressing on tough action, it’s time for India to assure the world that it is serious in maintaining the image of high quality.”
When Dr Lamba was asked whether the issues of spurious drugs and the government action against pharma companies indicate at some structural lacunae in the country’s pharma industry, he recalled the Mashelkar Committee on spurious drugs and drug-regulatory revamp which had submitted an interim report in 2003 to India’s then health minister.
The expert committee, chaired by Dr R A Mashelkar, was constituted to examine all aspects about India’s regulatory infrastructure and the problem of spurious/substandard drugs.
The panel, which recommended centralisation of the country’s drug-regulatory system and upgrading of the regulatory infrastructure, accused errant state drug authorities of being partly responsible for the entry of sub-standard drugs in the market, Dr Lamba said, adding that by vesting licensing with the federal government, the regulatory system could be bettered.
Suggesting ways ahead, the expert said a national drug authority could be set up at the federal level by upgrading the current Central Drugs Standards Control Organisation (CDSCO), which discharges functions assigned to the federal government.
“Although many legislative changes have since been carried out to improve the regulatory norms, upgrading of the infrastructure continues to be unfulfilled,” Dr Lamba said.

He added that among other recommendations made by Mashelkar Committee were a stringent punitive system for spurious drug-makers, including death penalty for those who cause harm to body to loss or life. It also advised that offences related to spurious drugs should be made cognizable and non-bailable.
“Even after 20 years these recommendations are yet to be implemented and it’s not surprising that we are seeing a repetition of the issues in quality and compliance of medicines regularly,” Dr Lamba said.
While India is often called the world’s pharmacy, it also faces the challenge of spurious drugs. Prices of drugs are also getting costlier in the country. Can India’s pharma industry be still called a patient-friendly one?
Dr Lamba, who has more than 30 years of experience in the pharmaceutical sector, believes while the industry is very friendly from the point of view of affordability, a lot needs to be done when it comes to compliance on quality and good manufacturing practices.
He said India has nearly 10,000 companies and that is quite a lot to manage. “This industry needs consolidation and fly-by-night operators who get easy licences need to be weeded out. Even today, 90 per cent of the business of pharmaceuticals in the Indian market comes from top 150 companies,” he told India Weekly.
He said India is the world’s largest provider of generic medicines and vaccines by volume and its exports meet the standards and requirements of highly regulated markets of the US, UK, European Union and Canada.
Since India has a federal functioning, regulatory mechanisms in implementing laws and guidance in the pharma sector could also be a key aspect to address.
Reflecting on that, Dr Lamba said drug regulation has been the focus of several recent policy reform efforts in India, starting with the Mashelkar Committee report to the Ranjit Roy Chaudhary Committee report in 2013.

But, the regulatory structure continues to be plagued with several challenges, including issues related to regulatory harmonisation between the federal government and states, access to regulatory resources, transparency that have undermined the general effectiveness of the regulatory system, he added.
“At this juncture, the Drugs and Cosmetics (Amendment) Bill, 2015 to amend the Drugs and Cosmetic Act, 1940, is expected to overhaul the drug regulation. A revised Schedule M as per Drugs and Cosmetics act is expected in 2023,” he said.
“Drug regulation is a public policy response to the demands of public health and the changing needs of pharmaceutical industry Thus, the objective of regulatory control is a question of achieving a ‘balance’ between protecting and promoting public health and facilitating the industry vis-à-vis compliance with regulatory standards. Consequently, although the regulatory objectives seem clear, the actual quantum of regulatory oversight, the mechanism for achieving regulatory compliance and the actions needed to deal with non-compliance have to be designed in a manner that is sensitive to the characteristics of the regulatory space.” Dr Lamba added.
Speaking on the functions of the federal and state governments, he said the main functions of the federal government include approval of new drugs; registration and control of imported drugs; approvals for clinical trials; laying down standards for drugs, cosmetics, diagnostics and devices; approval of licences for high risk products (large volume parenterals, vaccines and biotechnology products and operation of blood banks); co-ordinating activities of the states and advising them on matters of uniformity in regulatory administration in the implementation of the Drugs Controlling Authority.
“The state governments are responsible for licensing of manufacturing establishments and sale premises, undertaking inspections of such premises to ensure compliance with licence conditions, drawing samples for testing and monitoring of quality of drugs, taking actions like suspension/cancellation of licences, surveillance over sale of spurious and adulterated drugs, instituting legal prosecution when required and monitoring of objectionable advertisements for drugs. I see major issues in the SDRA as most of the small scale and medium scale manufacturing companies are under control of SDRAs and there is no uniform oversight and controls at SDRAs,” Dr Lamba added.
The adverse reports from overseas related to India-manufactured drugs have raised concerns over the credibility factor and according to Dr Lamba, the country’s pharma industry has faced several challenges that have affected its reputation as a reliable supplier of quality drugs.
“India has long been regarded as the “pharmacy of the world”, thanks to its thriving pharmaceutical industry that produces affordable generic medicines for the developing world. However, in recent years, India’s pharmaceutical industry has faced several challenges,” he said.
One of the main challenges that India’s pharmaceutical industry is facing, according to Dr Lamba, is the issue of quality assurance. The US Food and Drug Administration (FDA) raised concerns over the quality of drugs manufactured by some pharmaceutical firms and that has led to a slump in the number of Indian pharmaceutical companies receiving approvals from the FDA, resulting in loss of business for them.
Besides quality assurance, lack of investment in research and development and disruptions caused by the Covid-19 pandemic have also seen India’s below-par performance as a supplier of quality drugs and live up to its reputation as the world’s pharmacy, he added.
The Biocuris CEO, however, expressed optimism that the Indian government is taking steps to address the challenges and restore India’s position as a reliable supplier of quality drugs.
“While it is not an easy issue to handle but with political will of the government, improvement in drug control administration, strict enforcement of the law and harmonisation of quality standards as per PICS (Pharmaceutical Inspection Cooperation Scheme) can bring India’s glory as the world’s pharmacy back,” he added.
Finally, when asked about three steps that he feels India needs to take to improve its pharmaceutical sector vis-à-vis the world, Dr Lamba said a central drug authority must be made active with power for licensing and GMP across India.
His second suggestion was to implement a uniform code of marketing to prevent unethical practices of pharmaceutical companies, such as providing freebies and gifts to doctors to promote their drugs.
The Uniform Code for Pharmaceutical Marketing Practices (UCPMP), which the government put in place in 2015 to prevent unethical practices by the pharmaceutical firms, is currently voluntary.
Dr Lamba also called for strict provisions of law and enforcement, including cancellation of licences to weed out the industry’s black sheep.
“Offences related to spurious drugs should be made cognizable and non-bailable,” he said.
Dr Lamba has more than 33 years of proficiency in the pharmaceutical sector and led large teams across the globe in areas such as planning, execution and leadership. He has served at operational and leadership positions at companies such as MSD, Pfizer Ranbaxy, Dabur, Gland, Lupin, Eisai, among others. He has completed MPharm, PhD from Punjab University in Chandigarh, India, where he is based. Dr Lamba is currently associated with Biocuris pharmaceuticals, working as its CEO. He has been thrice honoured with a place in “100 of the Most Inspiring People” in the life science industry by PharmaVOICE, USA. He has been associated with bodies such as Indian Pharmaceutical Association and International Society for Pharmaceutical Engineers.